For years, corporate automation has been stuck in a frustrating cycle: IT rolls out new technology, but the promised efficiency gains never materialize because the tools are applied to broken business processes. Nowhere is that disconnect more apparent than in the healthcare industry. The sector has long been a technology laggard, where an estimated 80% of healthcare data is unstructured, trapped in antiquated formats that stymie automation. But AI is finally starting to break that logjam, creating possibilities where previous tech waves, like the cloud, fell short.
Abhijeet Vaidya, Practice Leader for Data & AI at healthcare digital transformation solutions provider Emids, has over two decades of experience, having architected solutions for some of the world's largest data ecosystems. He previously headed Data & Intelligence Delivery for North America Financial Services at Cognizant, leading 4,000 associates and managing a revenue target of over $300 million. For Abhijeet, the real barrier to automation isn't technology but how organizations are structured to use it.
"This isn't an AI question, per se," he states. "It's an issue of organizational structure, and it leads to the 'use case trap': departments develop use cases in isolation without ever thinking how it all comes together to deliver greater value." The consequence is particularly evident in healthcare, where automation initiatives optimize individual administrative tasks while broader workflows remain trapped in fragmented systems.
Straight outta 1998: The inefficiency is staggering, particularly in prior authorization workflows that still rely on technologies from the late 1990s. "For prior authorizations, 80% of the data is still exchanged through faxes, emails, and phone calls," Abhijeet notes. "There is so much inefficiency. With AI, we can automate that entire workflow. Whether information arrives as a fax, a phone call, or an email, the technology can read the document, transcribe the conversation, and convert that unstructured data into a structured format in our systems," he explains. "This allows us to complete the process in minutes, not days."
This kind of targeted improvement demonstrates AI's technical capability while revealing why automation alone isn't enough. The "use case trap" explains why so many automation efforts fail to deliver material value. By focusing on optimizing a single task within a departmental silo, such efforts risk reinforcing the very fragmentation that creates inefficiency.
A headcount headache: Abhijeet recounts the frustration a CIO expressed after a year-long automation initiative. "I talk to CIOs who say, 'I had 100 people, I ran automation for a year, and I still have 100 people, maybe 110. How do I get the benefit? It didn't materially impact licensing costs or operations costs, so where's the value?'" he recalls. The fragmentation becomes visible when examining a single patient transaction across departments. "In a typical prior authorization, one team captures the fax, another reviews it, and a third handles payment integrity. While these are all different departments working in silos, from the patient's perspective, it is all part of a single treatment journey," says Vaidya. Without coordination across these touchpoints, automation delivers incremental improvements rather than enterprise-wide efficiency.
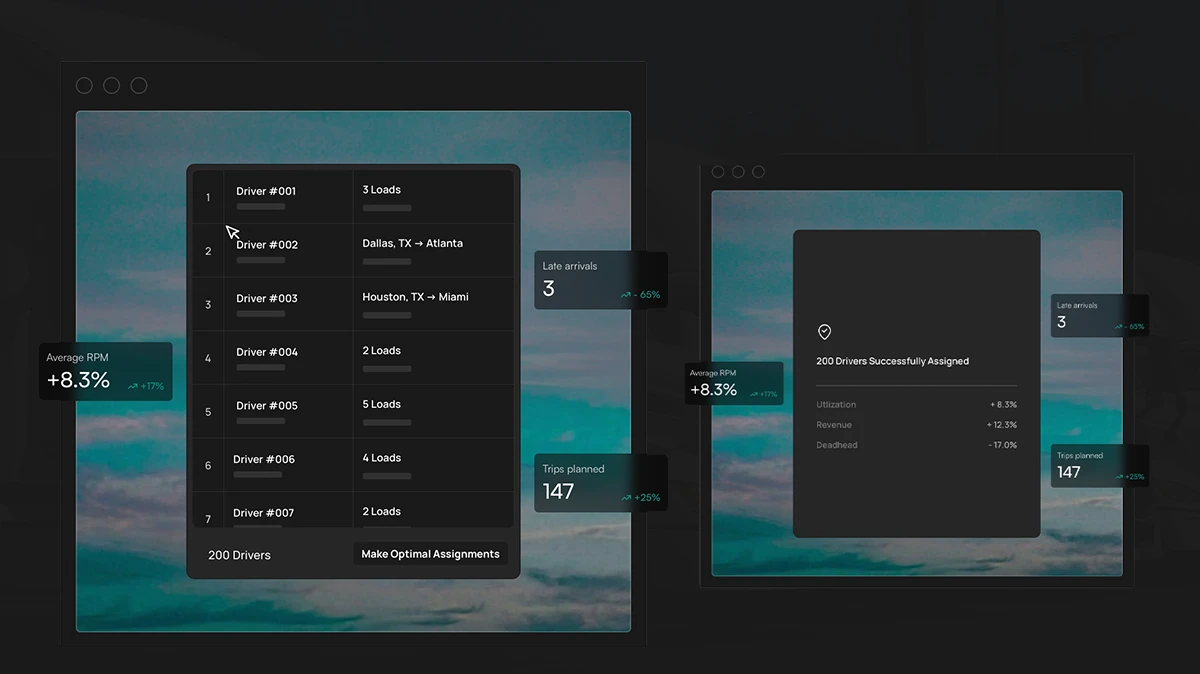
Climbing the ladder: So how does an enterprise escape the trap? Abhijeet says the answer lies in a strategic data platform that sequences AI adoption through a clear maturity model, providing the unified foundation needed to coordinate AI initiatives across departmental boundaries. It's a roadmap for everything from tooling and training, to the need for governance. "The first stage is AI-enabled, where you bring in AI to assist your teams. For a CIO, that could mean using AI to help developers write code faster and more compliantly," Abhijeet outlines. "The second is AI-first, where AI does the work and people act in an oversight role. And the third is AI-native, where AI is actually writing the software."
Abhijeet also injects a dose of realism, noting that scaling AI in a regulated field like healthcare is fraught with challenges. While some companies are already using AI assistants to reduce the administrative burden on doctors, success at scale requires acknowledging the need for human oversight, navigating strict regulatory requirements, and customizing solutions to specific workflows.
Governed and guarded: "Trying to force-fit a generic solution is like putting a square peg in a round hole. This is often when you see pushback emerge." This caution translates into a systematic checklist organizations must satisfy before deployment. "Health care is very regulated and heavily scrutinized, so we are going to take a cautious approach," he says. "Is the AI governed? Am I comfortable with it? Am I seeing a human in the loop if an exception happens? Are edge cases being addressed? There is that component. Are governance, compliance, and security all being handled?"
Abhijeet puts the challenge in sharp relief by contrasting the speed of modern financial transactions with healthcare’s current timelines. The disparity is stark enough that the federal government is now mandating faster turnaround times and facing pressure to enforce them. Initiatives from major insurers like Humana to reduce prior authorization requirements signal some forward momentum, but the government's mandated timeline reveals just how much ground the industry has to cover.
"When you apply for a credit card, it's approved in seconds. So why does it take seven days to approve a medical treatment?" Abhijeet asks. He notes that the seven-day figure is a federal mandate for 2027, not current reality. "Why don't we have a 'minutes mandate'?" he continues. "They set the bar at seven days because they know that we are nowhere near that."