Caught in the race to deploy AI, healthcare leaders could be overlooking the most valuable use case yet: a disjointed patient experience. Now, a new approach is quietly emerging, one focused on the less glamorous work of data integrity, thoughtful design, and a unified patient experience. But it's an innovation that can only move at the speed of trust, some experts say.
Joshua Hickey, a Principal Technical Product Manager at Mayo Clinic, is one of the pioneers charting this new direction in healthcare AI. With two decades of experience at companies like AT&T and Kaiser Permanente, Hickey now leads technology for an organization that engages two billion care seekers annually. For him, serving patients means rethinking everything, from journey mapping and user feedback to the definition of data itself.
Healthcare departments solving problems in silos create a disjointed patient journey, Hickey says. The fix is a process of journey mapping that orchestrates every touchpoint around holistic patient needs. Ultimately, the destination is a "Patient360" profile that treats patients as whole individuals.
Connecting the dots: The fragmentation isn't accidental, Hickey explains. It's the direct result of departments competing for separate funding pitches. "I think of healthcare as a continuous journey, not a set of disconnected steps. When departments try to solve things separately, the patient journey can feel fragmented. While these individual solutions are great, they shouldn't be prioritized individually. The patient's needs must be treated as a whole, as one continuous journey."
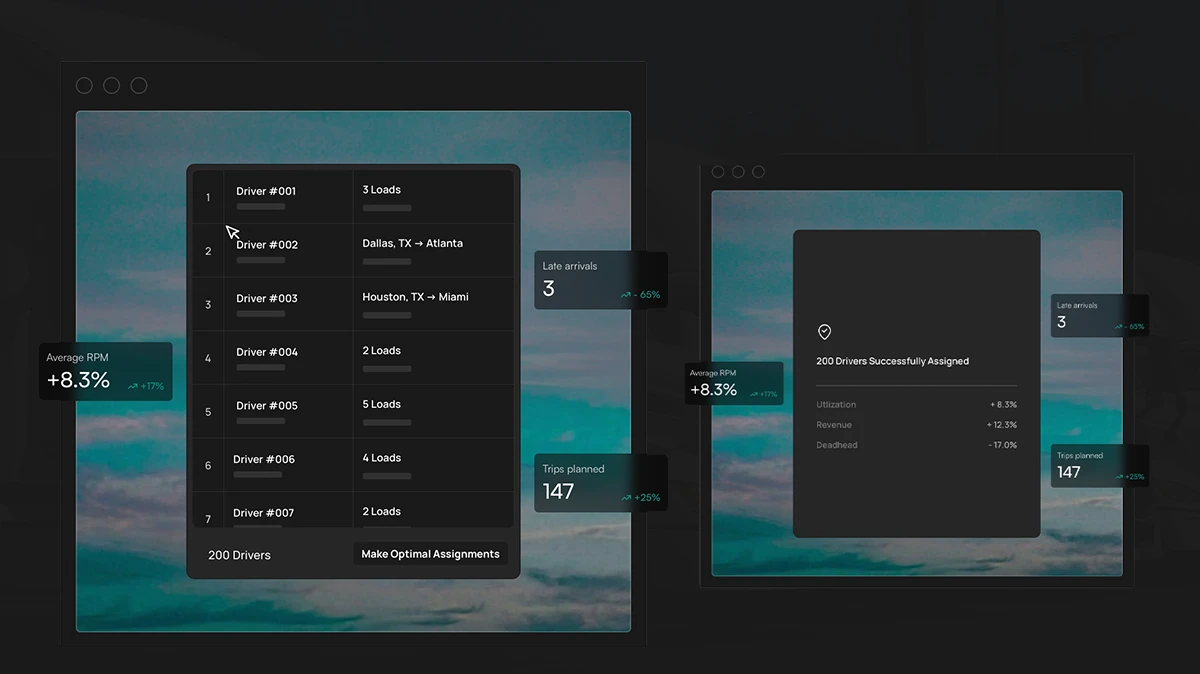
Hickey describes how, with analytics acting as the engine, sentiment can become a live feedback loop. For instance, if a patient bounces from a page, the system can remember and offer a better option on their next visit. This creates what Hickey calls a 'Netflix-like' experience, a concept further detailed in his work on designing for digital empathy.
From report to reflex: The old model is broken, Hickey argues. Reacting to analytics reports months later is simply too slow for an agile world. "These same insights must be treated as active feedback loops into our AI models, evolving beyond their traditional role as reactive KPIs for leadership reports. That's a bad way of doing business in an agile world with the power of AI."
The wrong game: Hickey challenges the entire premise of call center efficiency. The goal should be the complete elimination of user frustration instead. "It's the wrong game to play. That's processing tickets faster, and that's not the game that we really want to play. We want to allow the user to have self-service and schedule digitally."
The sound of silence: Instead, Hickey suggests a new purpose for call center data: feed it directly to the UI team for product improvement. "I want that feedback loop to go back into our UI and have it learn from the behavior of users who turn to the call center as a workaround. The goal is to achieve zero call-center calls for that user experience."
Tracking user behavior so closely requires absolute trust, Hickey says. But building that trust requires two things. The first is explicit patient consent with distinct controls for marketing versus clinical care. The second is a disciplined process for data validation. He calls the combined approach a 'supply chain of trust,' describing it as a rigorous validation of data from source to model. Get the balance wrong, and the entire system fails.
The secret sauce: While the industry chases complex algorithms, the real value is somewhere far less glamorous, Hickey says. "The models are a commodity. That skill set will be 100% constrained by the data they receive. The secret sauce is having amazing Epic interoperability and a refined process that is ready to automate. You've got to have good data going in."
The rule of thirds: Over-rotate on the UI or the AI hype, and you'll neglect the data foundation that makes it all work. "I look at it as a third of your time on the data, a third on AI model development, and a third on user research for the design. If you don't equally pay attention to all three, you might over-rotate on the user experience or the hype with AI and forget about the data, which is a third of the entire equation."
The payoff for an empathy-driven framework is a future of proactive, personalized healthcare. But for Hickey, the vision is also personal. "I have a Garmin device. I've had AFib, so I have an EKG monitor. I would love to hand that over to AI to mix with my EHR data and get some better analysis out of this. And if I am in AFib, I want to shoot that analysis over to get the physician's opinion on it and have that data set easily exchanged." It’s a future where our daily data integrates safely with clinical records, giving physicians tools for proactive care. Already, that vision is supported by the growing trend of patients wanting to share wearable data with their doctor, he says.
Staying realistic about the regulatory hurdles is essential, Hickey concludes. But so is staying clear on the ultimate goal: augmenting physician expertise with better, faster information. "You're not getting the final opinion. You're still curating what AI has suggested for the physician to make the decision on or further dive into. You're just finding this information more in real time, rather than letting it go unobserved."